 ...
... By Alexis KayserShareNewsweek is a Trust Project member
By Alexis KayserShareNewsweek is a Trust Project memberThis is a preview of the December 18 edition of Access Health—Tap here to get this newsletter delivered straight to your inbox on Thursday mornings.
Access Health will be taking a break for Christmas Day and New Year’s Day. Thank you for following along this year—I'll see you again on Thursday, January 8, 2026!
I’ve been thinking back on my conversations from the past year, as one does when it’s too cold to go outside without full winter PPE. Many of them revolved around a common theme: improving the patient experience.
What should this “patient experience” actually look like, though? What are we striving towards? This year, health systems have worked to improve the patient-physician relationship, deploying ambient scribes to allow for eye contact and make sure all concerns are thoroughly documented. Hospital-at-home programs and widespread telehealth deployment have given patients more control over where and when they receive care. AI agents in call centers, digital command centers to hasten triage and placement and improvements in medical record sharing have all worked to reduce friction for patients and treat them in a timelier manner. Pharmaceutical development has granted patients more treatment options than ever before, as has expanded access to clinical trials. Plus, genomic science is advancing, aiming to help identify the right therapies with less trial and error.
The year's most-talked-about “patient experience” indicators fit somewhere in that framework, I would argue. But recently, I had a conversation that really surprised me.
I was on a Zoom call with Dr. Kevin Pantalone, an endocrinologist and the director of diabetes initiatives at Cleveland Clinic. We were discussing the results of a recent study his team had conducted, which almost sounded too good to be true. Within a year, the Clinic reversed type 2 diabetes in 71 percent of the study’s variable group patients.
They did this without prescribing bariatric surgery, GLP-1s, keto diets or Equinox memberships. They basically prescribed good ol’ “diet and exercise.”
But there were two key departures from that traditional (dreaded) protocol, Pantalone said. During the trial, patients received highly personalized feedback and 24/7 support from an AI agent.
Cleveland Clinic used a platform from Twin Health to create “digital twins” of individual patients’ metabolisms. Frequent feedback from remote patient monitoring devices allows the twin to predict a person’s reaction to certain foods, activities and lifestyle habits. Patients track their behaviors and ask for advice in the Twin Health app, and their AI-agent “twin” will recommend modifications or changes to limit unfavorable biometric changes.
Even Pantalone was surprised by the results. Seventy-one percent of the patients using Twin Health’s intervention had achieved an A1C under 6.5 percent, effectively reversing their type 2 diabetes. Only 2.4 percent of the 50 patients receiving standard care from Cleveland Clinic saw the same result. More than half of Twin Health users were able to come off all their glucose-lowering medications except for metformin, compared to 2.8 percent in the standard care group, and Twin Health patients dropped body weight at around twice the rate of their peers, according to the study.
Now, this isn’t necessarily a scientific revelation. We’ve long known that a person’s behavior can directly and profoundly impact their biology.
But some physicians have the tendency to limit their patients, Pantalone told me—even subconsciously. When elderly, stubborn or highly symptomatic patients came into his office asking to come off medications, he told them there was no other option. Many of those same patients excelled using Twin Health’s intervention. They just needed a different kind of support.
“A lot of the patients that were enrolling in the study...I was skeptical,” he said. “They're 72 years old. They're not really tech-savvy.”
“What I learned through the study is that my own biases as a physician shouldn't dictate or determine what options I give my patient,” he continued. “Who am I to say, ‘I don't think you can do this?’ Give them the opportunity.”
I’d like to explore that facet of the patient experience more in the new year. Amidst all the simplifying and streamlining, where in the care process can we expand patients’ agency—not just their convenience?
If you’re interested in chatting about this, send me an email at [email protected]. I’d love to hear from you.
And if you’d like to read more about the Cleveland Clinic study, I recently published the full story on Newsweek. Click here to check it out.
In Other News
Major health care headlines from the week
- Sammie Mosier, senior vice president and chief nurse executive at HCA Healthcare, has died unexpectedly at the age of 50.
- The Nashville-based, for-profit health system announced the loss in a LinkedIn post on Tuesday.
- Mosier began her career at HCA Healthcare nearly 30 years ago at its Frankfort Regional Medical Center in Kentucky, working as a bedside nurse.
- HCA Healthcare described Mosier as a champion for nurses’ growth and development and a tireless advocate for their needs.
- “Sammie was a remarkable nurse leader whose passion for advancing nursing and supporting teams was felt far beyond the US...She was always inspiring and generous with her support and passionate about empowering nurses at every stage of their career,” Kathryn Hornby, chief nursing executive of HCA Healthcare UK, wrote on LinkedIn.
- The CDC officially rolled back recommendations that all healthy newborns receive the first hepatitis B vaccine within 24 hours of birth.
- This is a distinct departure from decades of vaccination precedent. The United States has been advising parents and clinicians to administer the vaccine in the infant’s first day—regardless of the mother’s hepatitis B status—since 1991.
- Now, the CDC recommends delivering the first dose “no earlier than two months of age.” The previous standard suggested administering that dose earlier. Even in infants who were not medically stable enough to receive it within 24 hours of birth, the CDC had long advised clinicians to give the initial injection at whichever benchmark came first: hospital discharge or 1 month of age.
- Some states, including New York, Connecticut, Illinois, Maine and New Jersey have declined to follow the new recommendations. Their state health departments will continue to advise clinicians to administer the dose within 24-hours as they have for 34 years, per the American Academy of Pediatrics’ (AAP) standard. Others—like California, Oregon and Washington—have formed regional coalitions to craft their own vaccine guidance based on recommendations from the AAP and other trusted physician associations.
- “Rolling back this recommendation creates confusion and doubt about vaccines, reverses hard-won progress in preventing hepatitis B, and will undoubtedly result in completely preventable illness and death,” the American Medical Association (AMA) said in a statement Tuesday evening.
- Meanwhile, the NIH lacks permanent leaders in 13 of its 27 institutes and centers, Reuters reported yesterday. The agency has been scrambling to fill the vacancies after losing longstanding talent to retirements, internal rearrangements and mass layoffs.
- Many of the open positions were posted with a two-week application window, ending November 7. But concerns about the tight timeline, the agency’s instability under the Trump administration and the overwhelming scope of the role may have deterred applicants, past and current leaders told the news organization. Several of the deadlines were extended to December 12, and the NIH has yet to release any selections.
- The AMA released a new analysis of health insurers’ footholds in U.S. metros, finding that a handful of payers have become “highly concentrated” and dominant in their respective markets. The report is 86 pages, so here’s a brief summary:
- Last year, at least one insurer held a commercial market share of 30 percent or greater in 91 percent of metro areas. A sole payer held at least half of the market share in 47 percent of metro areas.
- The five largest insurers by market share in 2024 were UnitedHealth Group (16 percent), Elevance Health (12 percent), Aetna (12 percent), Cigna (9 percent) and Health Care Service Corp. (8 percent). But if Blue Cross Blue Shield’s regional entities were combined in the analysis (rather than separated as, say, BCBS of Michigan and BCBS of Florida, which each held 2 percent of their area’s market share last year), they would dominate the field at 43 percent.
- Dwindling competition leads to higher premiums and fewer options for patients, AMA CEO Dr. John Whyte said in a statement.
- To learn more about how payer concentration impacts health systems, check out my recent Pulse Check interview with Banner Health CEO Amy Perry.
Pulse Check
Executive perspectives on key industry issues ...
...Quick! When you think of health care AI companies that dominated headlines in 2025, which name comes to mind first?
For me—and I imagine, for many of you—Abridge is at the top of the list. Their generative AI solutions are among the most popular on the market, with implementations across more than 200 health systems including Mayo Clinic, UChicago Medicine, UPMC and Northwell Health. The number of provider organizations that choose Abridge has just about doubled since the company announced its $250 million Series D investment in February.
Ambient scribing was Abridge’s initial claim to fame, but its offerings are ever-expanding. The company now offers generative AI tools specifically for emergency departments and ambulatory surgery centers, behavioral health care and payer-provider ecosystems.
Needless to say, Abridge’s CEO, Dr. Shiv Rao, has had a busy year. I connected with him this week to reflect on the company’s successes in 2025—and get a glimpse of what’s coming in 2026.
Abridge is up and running at more than 200 hospitals and health systems. What do you consider the key decisions that made that scale possible?
Abridge started from a simple belief: the heart of healthcare is the conversation between a clinician and a patient. As a doctor, I felt firsthand how documentation pulled me away from that moment, so we built technology that supports clinicians without disrupting that connection.
Our AI stays out of the way when it should, and steps in when it can meaningfully reduce the burden. We work closely with clinicians and health systems, listening to their needs and integrating into the workflows they already trust. That focus on usability, reliability, and genuine partnership is what allowed us to scale from an idea to a nationwide platform.
AI-powered clinical documentation is your company's claim to fame. But what are your ambitions beyond scribing?
This year alone, Abridge will support clinicians across more than 50 million conversations. Ambient AI has scaled faster than any other technology in the nearly two decades I’ve been a doctor, but we are just scratching the surface of what’s possible. We are building a system of real-time intelligence at the point of conversation that bridges across the entire healthcare ecosystem, including providers, payers, and patients. For example, we’re co-developing real-time prior authorization to empower clinicians to address payer requirements during the visit—not days or weeks later. We’re also developing embedded clinical decision support to help clinicians have all the information they need. At Abridge, our goal is to help the entire healthcare system save time, save money, and save lives.
CMS and commercial payers are moving toward prior auth modernization—faster turnaround times, electronic submission, gold-carding pilots. From your vantage point, what changes will actually move the needle for clinicians?
Imagine you’re in the exam room with your clinician who recommends you need an MRI. What if rather than having to play phone tag with the office and waiting weeks for prior authorization approval, it happens in real-time? That’s what Abridge is co-developing with Allegheny Health Network and Highmark Health—and will soon expand to other insurers and health systems. Abridge has the context of insurer requirements and is applying them throughout the conversation. Let’s say your clinician forgot to ask about pre-existing conditions, they would get a nudge to ask that question in real-time. The result? You can walk out with an approval. Transforming the prior authorization process from a few weeks to a few minutes is what will move the needle not just for clinicians but for patients who can get the care they need faster.
C-Suite Shuffles
Where health care leaders are coming and going- Humana announced a major hire on Tuesday, tapping Amazon’s Aaron Martin as its inaugural president of Medicare Advantage and a member of the insurance giant’s enterprise leadership team.
- Martin has served as Amazon’s health care vice president for more than three years, leading strategic partnerships and marketing for its health care vertical and overseeing its telehealth and chronic conditions products.
- Martin’s move to Humana is part of a larger succession plan. Current Insurance Segment President George Renaudin will retire by Q3 2026 after nearly three decades at the company, and Martin will take his place.
- At that time, John Barger—a 25-year Humana veteran currently serving as president of Medicaid and dual eligible programs—will assume Martin’s initial role as Medicare Advantage president.
- John Ryan will become the new chief strategy officer at Indiana University Health, effective January 1.
- He has spent the past four years as CEO of OrthoIndy, the largest orthopedic care provider in Indiana.
- Chicago-based CommonSpirit Health selected Kevin Fleming as its senior vice president of clinical service lines, reporting to Chief of Physician Enterprise Dr. Corey Karlin-Zysman.
- Fleming has held clinical leadership roles at prominent health systems across the nation, including Roper St. Francis Healthcare, Providence and—most recently—AdventHealth Central Florida.
Executive Edge
How health care execs are managing their own health ...
...When I was a kid, I cherished cozy snow days with my mom and sister, watching those cheesy Hallmark Christmas movies. If you’ve seen one, you’ve pretty much seen them all; they’re heavy on the tropes. Oftentimes, the "films" center on a busy corporate executive who bah-humbugs around the office, complaining about how the holiday season is interfering with productivity. They skip out on friendly gatherings and tear down the tinsel—until a hometown date, a secret Santa or an undercover elf reminds them of what they’ve been missing.
Most of us won’t snap out of our stress at the first sign of a sleigh bell, but those movies still serve as a good reminder—it's vital to take care of yourself during this period so you can show up for your organization, but also for your family and friends.
I was reminded of this yesterday during my interview with husband-and-wife duo Brian Schubring and Dr. Linda Schubring. Together, they run Leadership Vision Consulting, an executive coaching firm for teams and individuals. They’ve helped a number of health care executives manage their workload and recover from burnout over the years (I can vouch for this—I've verified the list of health care giants you would know, but can’t share it publicly).
From their home office in Minneapolis, Brian and Linda shared concrete tips on identifying and reducing symptoms of burnout as a high-ranking health care executive. I’ll share more from them in January 8’s edition of the newsletter, but for now, let’s focus on their tips for the holidays.
Editor’s Note: Transcription has been lightly edited for length and clarity.
Burnout can hit us in full force at the end of the year. Why does the pressure intensify in December, and how do Q4 stressors typically show up in health care executives?
Brian: Jokingly—but not so much—you're spending more time with your extended family. Every week when we’re coaching executives, people bring up the pressures they feel when their extended family gathers together. That is a unique disruption [from the routines of] the other 11 months of the year.
And if you're distant from your family, that also involves traveling during peak season, which adds additional stress.
Linda: And if you're close with your family, and your family doesn't understand what you do or the pressures that you are under, and are just relying on the news to tell them what's happening in the health care industry, it can feel even more profoundly lonely.
Brian: Also, there is an emotional expectation placed on people [during this time of the year] that's not necessarily there the rest of the year. Now, we're supposed to be joyful and happy and generous. That's not necessarily the emotional state that executives are occupying for the other parts of the year.
Your downtime is disrupted. You have to go to holiday parties. You're going to shows. You're going to different places during this time of year, instead of doing some of the self-care and rest that you may need.
Not to mention business deadlines and the fiscal year obligations that companies may have to their boards. All of these pressures are also funneling down towards those last few work days of the year, [placing] additional pressure on all the human systems that an executive is trying to keep together.
Linda: It feels more unique this year because it feels like the end isn't in sight. We're not going to pop a bottle of bubbly at the end of the year and just start with a clean slate. We will start the next year with the [same industry] pressures, and then some.
How do you recommend that leaders reconcile the social and professional pressures of the holiday season, neither of which they can just bow out of?
Linda: Not completely bow out of, but how can a team work together to create more boundaries? Maybe it's, “I’ll go for a couple hours, then I'll hand it off to a teammate for the last two hours.” Or, “Can you be my right-hand person? Can we do this together?” We find that when leaders are teaming up [to tackle big events], they feel a bond, and they feel like the loneliness or performance isn't just on them, but it is shared.
Brian: I often recommend lowering our expectations, just being realistic about the pressures we're facing and being able to say that out loud. Also, ask yourself what your best practices are in these situations. I was coaching an executive a couple of days ago, and he and his partner intentionally stay at a VRBO that's next to their parents’ house because they don't want to deal with the pressures of being in the home. They're still with the family, but they've created this healthy boundary where the two of them can connect and they can still be a part of the family system.
I’ll be back with more tips from the Schubrings on January 8. In the meantime, I wish you the happiest of holidays and a full cup to start the new year—whatever that looks like for you.
This is a preview of the December 18 edition of Access Health—Tap here to get this newsletter delivered straight to your inbox on Thursday mornings.
Request Reprint & LicensingSubmit CorrectionView Editorial & AI Guidelines Add Newsweek as a preferred source on Google to see more of our trusted coverage when you search.
Add Newsweek as a preferred source on Google to see more of our trusted coverage when you search.Recommended For You
 NewsTrump Just Issued a Major Marijuana Executive Order—Here’s What Changes6 min read
NewsTrump Just Issued a Major Marijuana Executive Order—Here’s What Changes6 min read HealthNew Medicaid Work Requirements Rolling Out For First Time In US4 min read
HealthNew Medicaid Work Requirements Rolling Out For First Time In US4 min read HealthNew York To Change Law On Assisted Dying6 min read
HealthNew York To Change Law On Assisted Dying6 min read Health CareCleveland Clinic Is Reversing Type 2 Diabetes—With AI, Not GLP-1s15 min read
Health CareCleveland Clinic Is Reversing Type 2 Diabetes—With AI, Not GLP-1s15 min read Health CareHarvard Med exec: Private dollars can’t fill federal funding gaps15 min read
Health CareHarvard Med exec: Private dollars can’t fill federal funding gaps15 min read NewsHow Health Care Plans Compare Ahead of Key Obamacare Vote5 min read
NewsHow Health Care Plans Compare Ahead of Key Obamacare Vote5 min readRelated Podcasts
Top Stories
 NewsEpstein Photos: Woman With ‘Lolita’ Quotes Written On Her Body Seen in New Images, As Files Deadline Approaches — Recap2 min read
NewsEpstein Photos: Woman With ‘Lolita’ Quotes Written On Her Body Seen in New Images, As Files Deadline Approaches — Recap2 min read U.S.Brown Mass Shooting Update: Person of Interest Identified — Report4 min read
U.S.Brown Mass Shooting Update: Person of Interest Identified — Report4 min read For MembersNewsUncommon Knowledge: The Quiet Promise That Could Define Trump’s 20264 min read
For MembersNewsUncommon Knowledge: The Quiet Promise That Could Define Trump’s 20264 min read NewsPam Bondi Issued Impeachment Ultimatum Ahead of Epstein Files Deadline5 min read
NewsPam Bondi Issued Impeachment Ultimatum Ahead of Epstein Files Deadline5 min read NewsDonald Trump’s Patriot Games Spark Hunger Games Comparison4 min read
NewsDonald Trump’s Patriot Games Spark Hunger Games Comparison4 min read NewsGreg Biffle, Family Dead After North Carolina Plane Crash2 min read
NewsGreg Biffle, Family Dead After North Carolina Plane Crash2 min readTrending
 FlagFlags Ordered To Fly at Half-Staff Across 6 US States Today5 min read
FlagFlags Ordered To Fly at Half-Staff Across 6 US States Today5 min read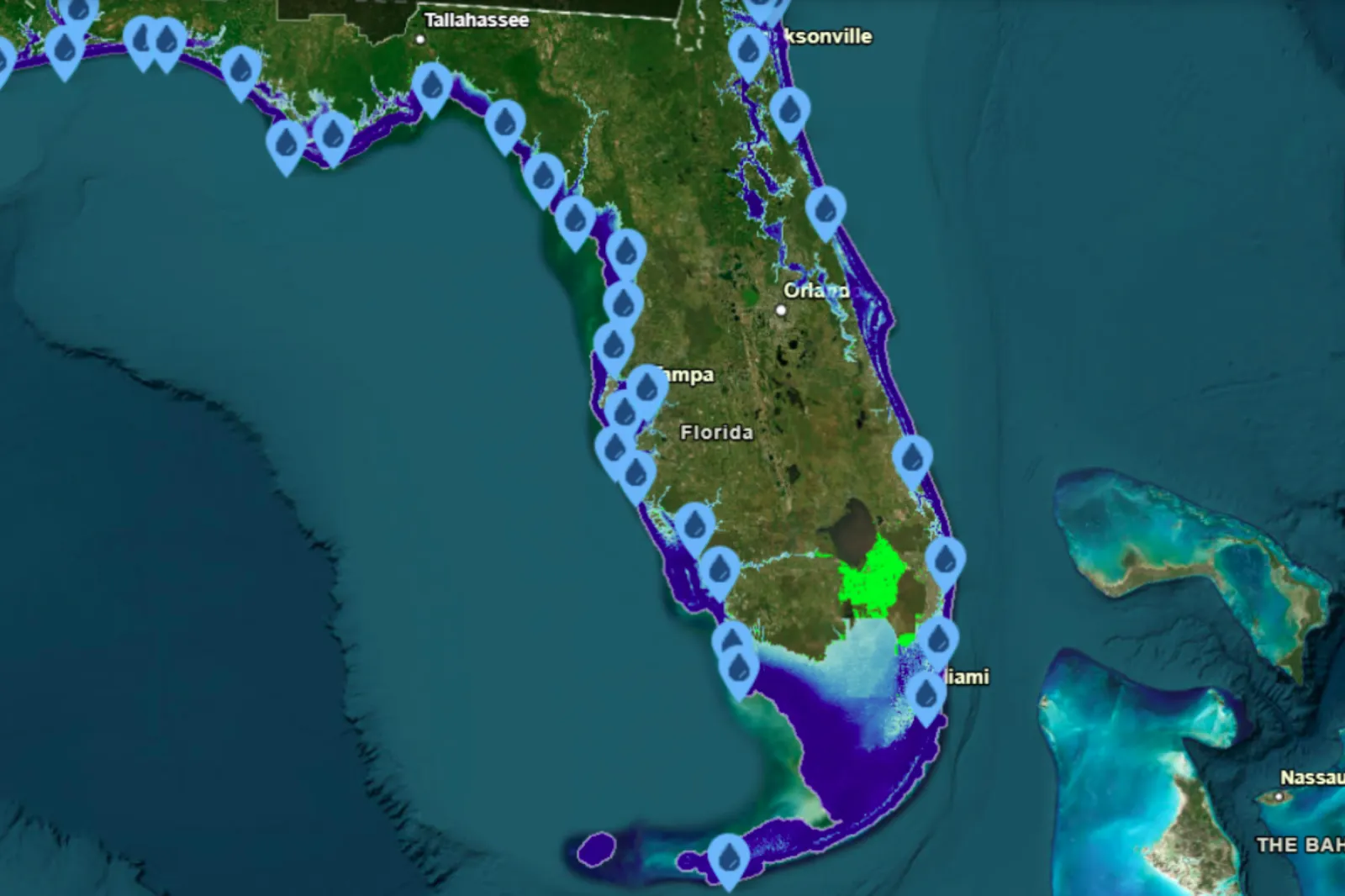 FloridaFlorida Map Shows Cities That Could Go Underwater if Sea Levels Rise5 min read
FloridaFlorida Map Shows Cities That Could Go Underwater if Sea Levels Rise5 min read DogsWatch the Exact Moment Dog Realizes He’s Never Going Back to the Shelter4 min read
DogsWatch the Exact Moment Dog Realizes He’s Never Going Back to the Shelter4 min read Donald TrumpDonald Trump Offered $250M to Run for a Third Term4 min read
Donald TrumpDonald Trump Offered $250M to Run for a Third Term4 min read SnowWinter Storm Warning As 16 Inches of Snow To Strike: ‘Impossible’4 min read
SnowWinter Storm Warning As 16 Inches of Snow To Strike: ‘Impossible’4 min readOpinion
 OpinionThe World Failed Holocaust Survivors at Bondi Beach | Opinion5 min read
OpinionThe World Failed Holocaust Survivors at Bondi Beach | Opinion5 min read OpinionMake-A-Wish Co-Founder: Healing Communities for 45 Years, One Wish at a Time | Opinion5 min read
OpinionMake-A-Wish Co-Founder: Healing Communities for 45 Years, One Wish at a Time | Opinion5 min read For MembersOpinionConventional Wisdom: The Susie Wiles Tell-All Edition4 min read
For MembersOpinionConventional Wisdom: The Susie Wiles Tell-All Edition4 min read OpinionMore ‘Gun Control’ Is Not the Answer | Opinion6 min read
OpinionMore ‘Gun Control’ Is Not the Answer | Opinion6 min read OpinionThe Bondi Beach Terror Attack Must Strengthen, Not Shatter, Our Bridges | Opinion5 min read
OpinionThe Bondi Beach Terror Attack Must Strengthen, Not Shatter, Our Bridges | Opinion5 min read